Int.J.Curr.Microbiol.App.Sci (2018) 7(11): 3264-3268
3264
Original Research Article https://doi.org/10.20546/ijcmas.2018.711.376
Bacteriological Profile and Antibiotic Sensitivity Pattern of Neonatal Sepsis
in a Tertiary Care Hospital
Pavneet Kaur* and Sarbjeet Sharma
Department of Microbiology, Sri Guru Ram Das Institute of Medical Sciences and
Research, Amritsar, India
*Corresponding author
A B S T R A C T
Introduction
Neonates with low immunity, always need
prolonged hospitalization which is a risk
factor of post-infectious complications.
(Adams-Chapman and Stoll, 2002) It is
estimated that about 5 million neonatal deaths
occur in a year out of which 98% occur in
developing countries. (WHO, 1996) Medical
advancements of the last twenty years have
increased the survival rate of neonates. Most
common causative bacteria in developed
countries includes Coagulase-negative
staphylococcus and group B Streptococcus
while in developing countries are E. coli,
Klebsiella, Enterobacter etc. (Waheed et al.,
2003) Klebsiella and Enterobacter species are
often associated with the production of
extended-spectrum beta-lactamase (ESBL)
among the multiresistant Gram-negative
bacteria. (Karunasekera and Pathirana, 1999)
The control of these hospital acquired
infections has been a challenging task.
(Goldmann et al., 1983) Spectrum of
International Journal of Current Microbiology and Applied Sciences
ISSN: 2319-7706 Volume 7 Number 11 (2018)
Journal homepage: http://www.ijcmas.com
India accounts for 30% of neonatal deaths globally. Bacterial sepsis is a significant cause
of morbidity and mortality in newborns. The study helps to make antibiotic policy in
neonatal sepsis. The main objective is to study the incidence of multidrug resistant gram
negative and gram positive organisms causing neonatal septicemia and their antibiotic
sensitivity pattern. The study was conducted in the Department of Microbiology over a
period of one year. Sample of blood was collected under aseptic precautions and processed
by standard techniques. Microorganisms were identified by Gram staining, standard
biochemical tests and appropriate antibiograms. The common microorganisms responsible
for neonatal sepsis were identified, and the resistant strains were studied. After
identification and antibiotic susceptibility testing, beta-lactamases were detected as per
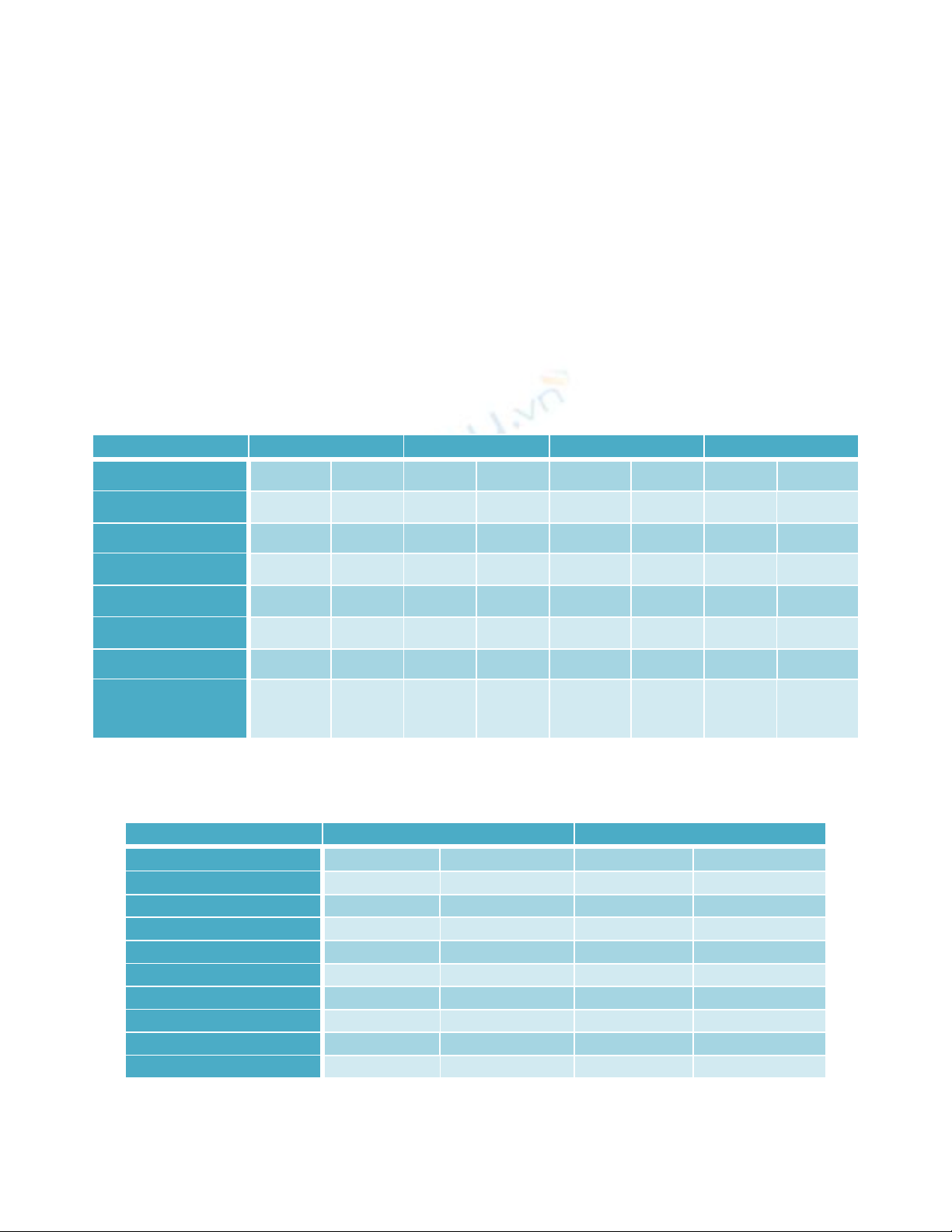
CLSI guidelines. In 233 blood cultures 18.9 % (44/233) culture positivity was seen. Out of
them, 31 (70.5%) were Gram negative and 13(29.5%) were Gram positive. Klebsiella
pneumoniae subspecies pneumoniae (45.5%) was the most common isolate. ESBL
producers were maximum (54.8%.) 25.8% of the isolates were positive for AmpC
production. The diverse microbiological pattern of neonatal septicaemia demands the need
for review of neonatal sepsis. The evaluation of the pathogens and their antibiotic
susceptibility is a relevant guide in the antibiotic therapy.
Keywords
Neonate, Blood
culture, ESBL,
AmpC, GNB
Accepted:
26 October 2018
Available Online:
10 November 2018
Article Info