Can Tho Journal of Medicine and Pharmacy 9(6) (2023)
106
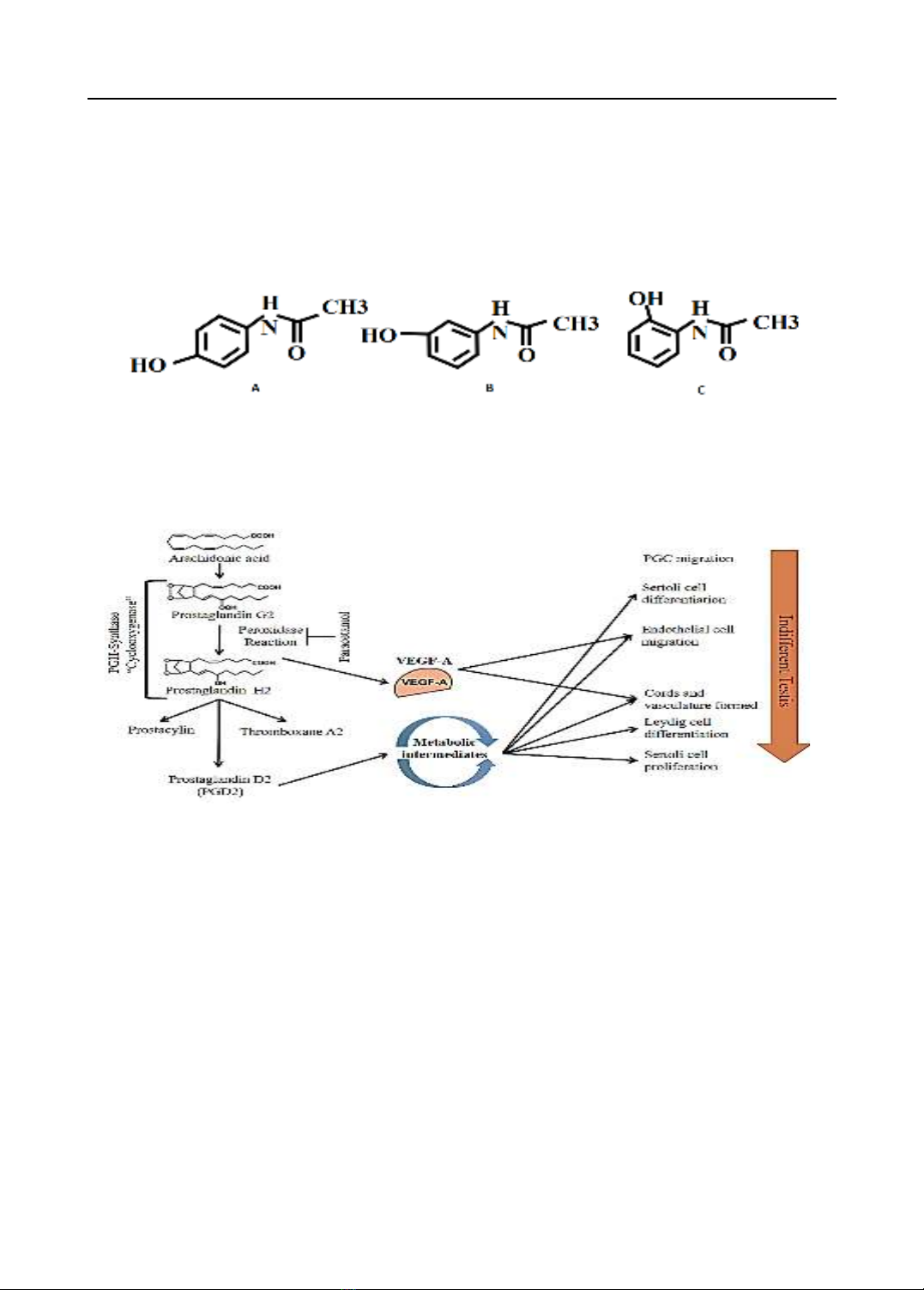
A REVIEW OF PARACETAMOL: MECHANISM OF ACTION AND
THE EFFECTS ON SPERMATOGENESIS
Huynh Thi Thu Hien, Nguyen Hoang My Duyen, Nguyen Hoang Anh,
Huynh Quang Hao, Nguyen Hoang Tin*
Can Tho University of Medicine and Pharmacy
*Corresponding author: nhtin@ctump.edu.vn
Received: 23/05/2023
Reviewed:14/6/2023
Accepted: 28/08/2023
ABSTRACT
Nowadays, there are many factors causing the decrease of male reproductive function such
as diet, routine, chemical, ... But some of them have not been paid appropriate attention to, especially
the use of paracetamol, which has a significant negative effect on the reproductive process. In this
study, we will summarize the results of several studies on the harmful effects of prolonged high-dose
use of paracetamol on sperm number, quality, portability and testicular morphology in experimental
animals and humans. The association between the long-term usage of paracetamol in chronic human
diseases and their toxicity is highly concerned, especially the reproductive function. Their toxicity
has increased more in adult male subjects, along with the introduction of studies on the use of high
and long-term doses of paracetamol affecting reproductive quality. This review discusses the link
between long-term usage of high doses of paracetamol and fertility as well as the effects of sex
hormones in experimental animals and humans nowadays. As a result, paracetamol affects the
reproductive system, impairing spermatogenesis and sperm quality. The amount of reproductive
function damage, the dosage and duration of paracetamol usage are closely correlated. When groups
of participants take paracetamol, numerous investigations in both experimental animals and humans
have shown a decrease in sperm count and sperm motility as well as abnormalities in sperm
morphology and testicular histology. Physicians have to exercise caution while treating patients with
paracetamol and other related medications, especially men. Therefore, more studies should be done
to determine the relationship between dosage, response, and treatment duration. When treating
patients with decreased sexual function, medications that can prevent paracetamol toxicity should
be used in conjunction with other medications. Especially, traditional medicine continues to play a
significant part in the research and development of many new medicines despite the rapid
advancement of contemporary medicine.
Keywords: paracetamol, spermatogenesis, testosterone, testis, infertility.
I. INTRODUCTION
Paracetamol (acetaminophen) is a common and widely used analgesic and antipyretic
medicine that is available without a prescription in both mono- and multi-component
combinations. It is the medicine of choice for patients who cannot be treated with non-
steroidal anti-inflammatory drugs (NSAIDs), such as those with bronchial asthma, peptic
ulcer disease, hemophilia, salicylate-sensitized people, children under the age of 12,
pregnant women or breastfeeding women [1]. Not only in the hospital but also in life, the
popular use of paracetamol also appeared with the aim of treating pain relief of acute diseases
such as abdominal pain, headache, toothache, traumatic pain, etc., and is also suggested in
the first treatment of chronic diseases such as osteoarthritis, degenerative spine, and spinal
pain [2]. However, in recent years, the benefits of using paracetamol for chronic diseases
have been questioned. Several studies have reported the toxicity of this drug with long-term