THAI BINH JOURNAL OF MEDICAL AND PHARMACY, VOLUME 16, ISSUE 2 - MARCH 2025
56
EFFECTIVENESS OF ULTRASOUND-GUIDED MDs SHOULDER
INJECTION IN THE TREATMENT OF SUPRASPINATUS TENDONITIS AT
THAI BINH MEDICAL UNIVERSITY HOSPITAL
Duong Thi An1*, Nguyen Duy Cuong1, Pham Thi Thanh Huyen1
1. Thai Binh University of Medicine and Pharmacy
*Corresponding author: Duong Thi An
Email: Dr.anytb@gmail.com
Received date: 02/3/2025
Revised date: 20/3/2025
Accepted date: 23/3/2025
ABSTRACT
Objective: To evaluate the results and safety of
ultrasound-guided MDs shoulder injection in the
treatment of supraspinatus tendonitis at Thai Binh
Medical University Hospital.
Method: Descriptive, longitudinal, non-controlled
study. Each patient received 2 ml of MDs Shoulder
collagen (1 vial per session) injected into the
subacromial bursa under ultrasound guidance, for
a total of 5 consecutive injections, one week apart.
The parameters to evaluate the effectiveness of
MD Shoulder collagen injection therapy include
improving pain levels on the VAS scale, improving
shoulder joint motor function on the OSS scale,
abduction angle of shoulder and ultrasound
imaging. Parameters to evaluate the adverse
effects of the therapy. Firstly, local manifestations
include increased pain after injection, infection at
the injection site, bleeding. Secondly, whole body
manifestations include changing in pulse and
blood pressure, headache, dizziness, nausea,
vomiting, itching, shock. Assessment time points:
pre-treatment (T0), 1-week post-treatment (T1),
4 weeks post-treatment (T4), and 12 weeks post-
treatment (T12).
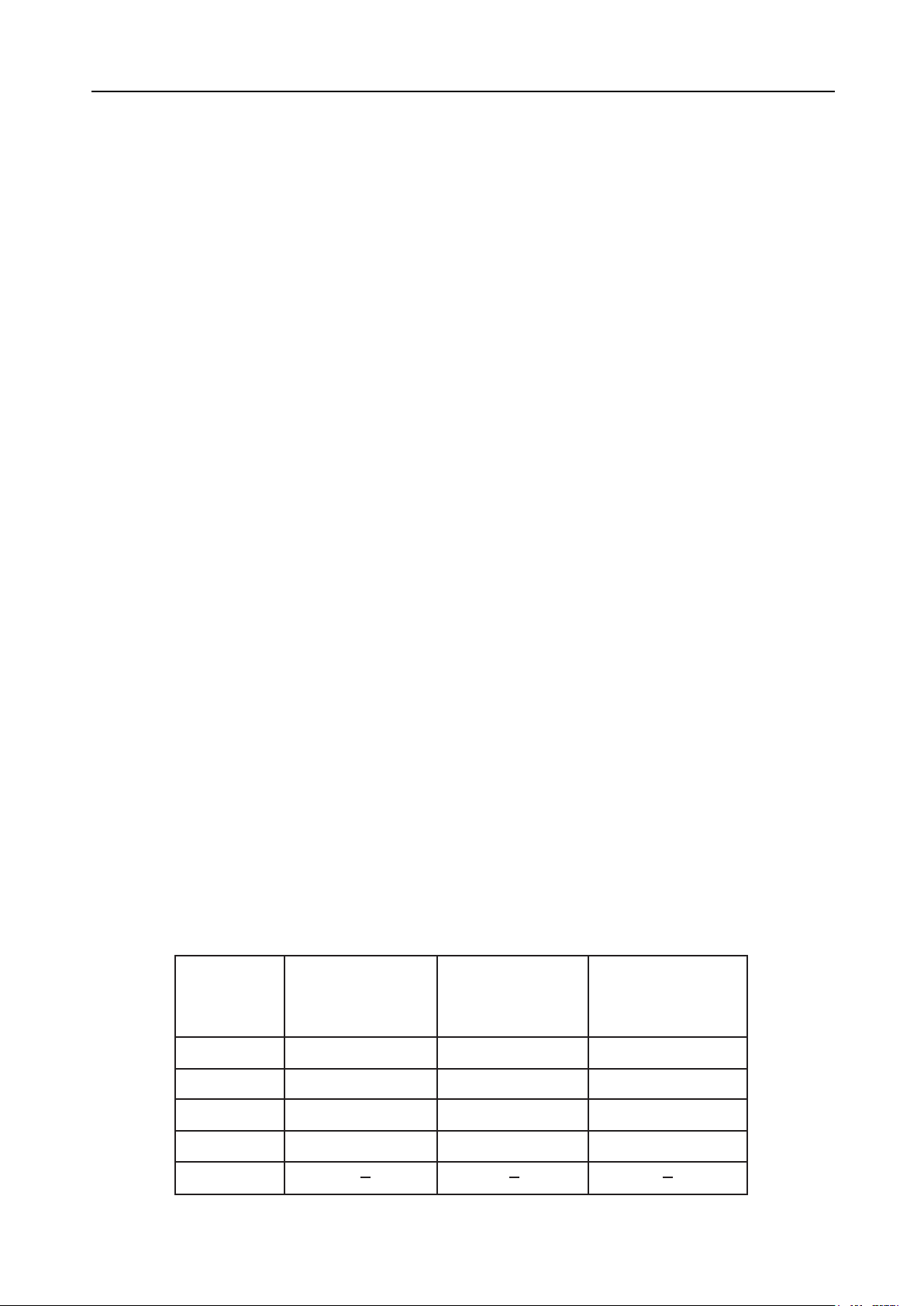
Results: The therapy of ultrasound-guided MDs
shoulder injection for supraspinatus tendonitis
obtained the following results: the therapy improves
VAS pain scores from week 4 and week 12, OSS
function scores from week 4 and week 12, abduction
angle of shoulder from week 1, week 4, and week
12; reduces hypoechoic rate on ultrasound by
week 12. Regarding adverse effects, no whole-
body adverse effects or serious complications were
observed during the 3-month follow-up. Increased
pain at the injection site occurred in 11.4% of cases.
Conclusion: The therapy of ultrasound-guided
MDs shoulder injection for supraspinatus tendonitis
obtained the following results: the therapy improves
VAS pain scores from week 4 and week 12, OSS
function scores from week 4 and week 12, abduction
angle of shoulder from week 1, week 4, and week
12; reduces hypoechoic rate on ultrasound by
week 12. Regarding adverse effects, no whole-
body adverse effects or serious complications were
observed during the 3-month follow-up. Increased
pain at the injection site occurred in 11.4% of cases.
Keywords: Effectiveness, MDs Shoulder,
ultrasound-guided injection, supraspinatus tendonitis.
I. INTRODUCTION
Rotator cuff tendon pathology is common. The
incidence of symptomatic or asymptomatic rotator
cuff disease, identified by surgery or imaging,
increases with age, from 9.7% in those under 20 to
62% in those over 80 [1]. In the general population,
rotator cuff pathology is the most common cause
of shoulder pain. Any rotator cuff tendon can be
damaged, but the supraspinatus tendon is most
frequently affected. The term “supraspinatus
tendon pathology” refers to primary damage to
the supraspinatus tendon, including inflammation
or degeneration, also known as “supraspinatus
tendonitis.”
There are various treatment options for
supraspinatus tendonitis. Local collagen injection
has been increasingly used in recent years,
particularly with ultrasound guidance. Under real-
time imaging, ultrasound-guided injection allows
for more accurate targeting of the damaged area
and needle placement.
Worldwide, studies have evaluated the efficacy of
ultrasound-guided collagen injection in the treatment
of shoulder joint pathologies. In 2014, Nestorova R
et al [2] published a clinical and ultrasound study
on the efficacy of Guna MDs collagen injection in
treating acute pericapsular shoulder inflammation.
The results showed significant pain relief, which
persisted after treatment ended. Shoulder function
improved, with a statistically significant difference,
and no adverse effects were recorded. Conclusion:
GUNA MDs collagen reduces pain and inflammation
significantly in patients with pericapsular shoulder
syndrome, subacromial bursa inflammation, and
improves shoulder function, thereby enhancing
quality of life.
In Vietnam, a study by Dang Chi Hieu and Nguyen
Vinh Ngoc [3] published in 2021 evaluated the