Hyponatremia
Definition: Hyponatremia is defined as a plama [Na+] < 135 mEq/L.
Etiology: Any process that limits the elimination of water or expands the volume
around a fixed Na+content may lead to a decrease in Na+ concentration.
-Expansion of the space surrounding the Na+ content:
+Pseudohyponatremia: a high content of plasma proteins and lipids expands the
nonaqueous portion of the plasma sample, leading to an errant report of a low ECF
[Na+].
+Hyperosmolar hyponatremia: an osmotically active solute other than Na
accumulates in the ECF, drawing water into the ECF and diluting the Na+ content.
Common causes: hyperglycemia (resulting in a fall in plasma [Na+] of 1.6 to 2.4
mEq/L for every 100 mg/dL rise in plasma glucose), post-transurethral resection
of the prostate (post-TURP) syndrome (glycine, mannitol, or sorbitol, can be
absorbed into the ECF during bladder irrigation)

+Rarely, the ECF water content rises simply because the ingested quantity of
water exceeds the physiologic capacity of water excretion in the kidney as in
psychogenic polydipsia, water intoxication from poorly conceived drinking games,
beer potomania, and the so-called “tea and toast” diet.
-“Appropriate” ADH secretion occurs with a fall in effective circulating volume.
In these conditions, thirst and water retention is stimulated, protecting volume
status at the cost of the osmolar status. This category is classically subdivided
based on the associated assessment of ECF status.
+Hypovolemic hyponatremia may result from any causes of net Na+ loss.
+Hypervolemic hyponatremia occurs in edematous states such as congestive heart
failure (CHF), hepatic cirrhosis, and severe nephrotic syndrome. Despite the
expanded interstitial space, the circulating volume is reduced. Alterations in
Starling forces contribute to this apparent paradox, shifting fluid from the
intravascular to interstitial space.
-“Inappropriate” secretion of ADH is characterized by the activation of
waterconserving mechanisms despite the absence of osmotic or volume-related
stimuli.
+Syndrome of Inappropriate ADH (SIADH)

Common causes: neuropsychiatric disorders (e.g., meningitis, encephalitis, acute
psychosis, cerebrovascular accident, head trauma), pulmonary diseases (e.g.,
pneumonia, tuberculosis, positive pressure ventilation, acute respiratory failure),
and malignant tumors (most commonly small cell lung cancer).
Diagnose:
o
Hypo-osmotic hyponatremia
Urine osmolality > 100 mOsm/L
Euvolemia
The absence of conditions that stimulate ADH secretion,
including volume contraction, nausea, adrenal dysfunction, and hypothyroidism .
-Pharmacologic agents may also stimulate inappropriate ADH secretion. Common
culprits include antidepressants (particularly selective serotonin reuptake
inhibitors [SSRIs]), narcotics, antipsychotic agents, chlorpropamide, and
nonsteroidal anti-inflammatory drugs (NSAIDs).
-Reset osmostat: the set point for plasma osmolality is reduced, occurs in almost
all pregnant women and occasionally in those with a chronic decreased effective
circulating volume.

Diagnosis
Clinical Presentation
-The symptoms are primarily neurologic
+Acute hyponatremia (i.e., developing in <2 days): nausea and malaise, further
symptoms is headache, lethargy, confusion, and obtundation, stupor, seizures, and
coma may occur as the plasma [Na+] falls acutely below 115 mEq/L.
+Chronic hyponatremia (>3 days' duration): symptoms and the increase in ICF
volume is minimized.
Diagnostic Testing:
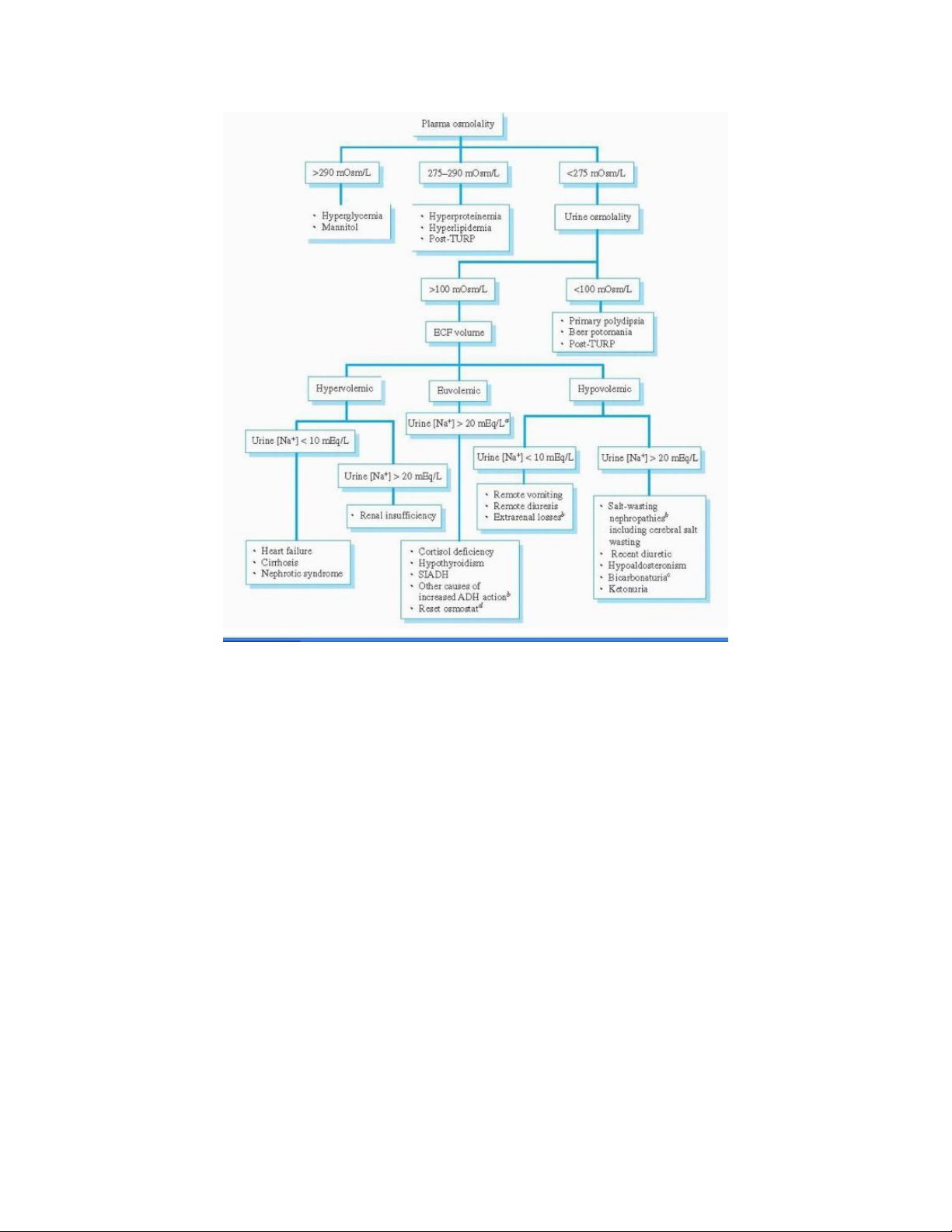
aUrine [Na+] may be <20 mEq/L with low Na+ intake
cFrom vomiting-induced contraction alkalosis or proximal renal tubular acidosis
dUrine osmolality may be <100 mOsm/L after a water load


























